Introduction
- An overuse injury characterized by pain on the outside part of the knee
- Pain can be experienced during activity or at rest with the knee bent
- Common in runners but also seen in hikers and cyclists
- Pathology
- Some debate over ‘friction’ and exact pathology
- Likely some inflammation/irritation of connective tissue on the outside of the knee
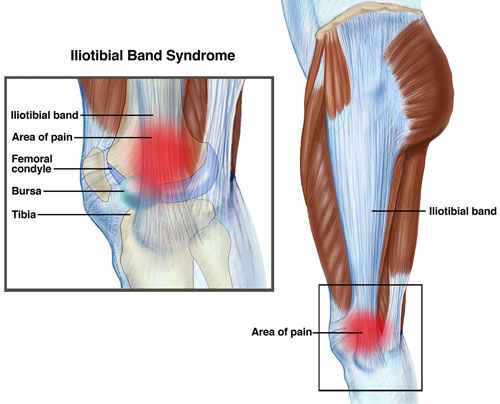
- Anatomy
- ITB attached to gluteus max and tensor fascia latae (TFL), runs along the length of the femur and attaches to the lateral condyle of the tibia
- Contributes to lateral knee stability
- *Very unlikely to be able to stretch it*
- May behave like a tendon in storing and releasing energy
- Potential most vulnerable range is 30-40 degrees of knee flexion when ITB may cross lateral femoral condyle
Unmodifiable Intrinsic Risk Factors
- Age
- Gender – although yet to be proven it is thought females have a higher likelihood of developing ITBS due to anatomical differences
- Genu varum (Bow leggedness)
- May overlap with anterior knee pain/patella femoral pain syndrome
Modifiable Intrinsic Risk Factors (*Best evaluated by a Physiotherapist*)
- Reduced control of hip adduction/internal rotation
- Reduced glute med strength
- Biomechanical abnormalities – foot alignment/pronation
- Weight (Increased BMI)
- Muscle imbalance and inflexibility
- Leg length discrepancy (LLD)
- A true LLD can be modified with appropriate foot lift orthotic
- A functional LLD can be modified with better muscular control and/or orthotics if necessary
Extrinsic Risk Factors (*Best evaluated by an MPT Physiotherapist*)
- Change in loading
- Return to running or activity after a break
- Training errors
- Change in training type (i.e. increased downhills for runners and hikers)
- Increase in training volume/intensity too quickly
- Change in training duration
- Increase in training frequency
- Change in weekly distance
- Running style
- Narrow step width
- Slower cadence
- Footwear – if not supportive enough to prevent over pronation
Treatment…To Be Continued.
***Book with MPT today to start your 1 on 1 individually tailored rehab program to get you back to what you love!***
Resources
Brindle, R. A. (2018). Physiological and Biomechanical Factors Contributing to the Hip Adduction Angle in Female Runners (Doctoral dissertation, Drexel University).
Fairclough, J., Hayashi, K., Toumi, H., Lyons, K., Bydder, G., Phillips, N., … & Benjamin, M. (2007). Is iliotibial band syndrome really a friction syndrome?. Journal of Science and Medicine in Sport, 10(2), 74-76.
Fredericson, M., & Wolf, C. (2005). Iliotibial band syndrome in runners. Sports Medicine, 35(5), 451-459.
Fredericson, M., Cookingham, C. L., Chaudhari, A. M., Dowdell, B. C., Oestreicher, N., & Sahrmann, S. A. (2000). Hip abductor weakness in distance runners with iliotibial band syndrome. Clinical Journal of Sport Medicine, 10(3), 169-175.
Tiu, T., & Craig Van Dien, M. D. Knee overuse disorders.
Meardon, S., & Miller, R. H. A new approach to iliotibial band syndrome in runners.
Meardon, S. A., Campbell, S., & Derrick, T. R. (2012). Step width alters iliotibial band strain during running. Sports biomechanics, 11(4), 464-472.
Miller, R. H., Lowry, J. L., Meardon, S. A., & Gillette, J. C. (2007). Lower extremity mechanics of iliotibial band syndrome during an exhaustive run. Gait & posture, 26(3), 407-413.
Nielsen, R. O., Nohr, E. A., Rasmussen, S., & Sørensen, H. (2013). Classifying running‐related injuries based upon etiology, with emphasis on volume and pace. International journal of sports physical therapy, 8(2), 172.