Resistance training is a popular form of exercise for weekend warriors and elite athletes alike. Unfortunately for some this passion can lead to many injury complaints. Research has found that 36% of injuries in the weight lifting population occur at the shoulder complex1. Some of the most common movements at the gym eliciting shoulder pain include the chest press, chest flies, shoulder press, lat pull down, push-ups and power clean. This pain can start off as a nagging pain during lifting but can progress into a constant shoulder pain and even pain at night. It is important to recognize and address shoulder pain with lifting early on to avoid more serious injuries and prolonged time away from the gym.
The cause of shoulder pain in lifters is often multi-factorial. Potential causes include training errors (rapid increase in training load, frequency, duration), poor technique, previous injury, poor rest, nutrition etc..
The pathology of shoulder pain with lifting also varies greatly. Sub-acute injuries include rotator cuff tendinopathies, long head bicep tendinopathy, glenohumeral joint instability, and distal clavicle osteolysis. Acute injuries include biceps and pectoralis tears and shoulder dislocations. We will dive into each one of these pathologies and how it affects our ability to perform lifts.
Rotator Cuff/Bicep Tendinopathies
The role of the tendon is to transfer force generated from muscle to bone. All tendons require a healthy load/capacity relationship whereas the tendon capacity exceeds the muscle load. If the tendon capacity is reduced (deconditioning/atrophy) or the load demand increases (higher volume or intensity of load) the tendon begins to fail which leads to a cascade of negative events referred to as a tendinopathy. You can think of a tendinopathy as a swollen, grumpy tendon that is irritable to load.
Tendinopathies can develop chronically or acutely. Acute development of tendinopathy (reactive tendinopathy) occurs when there is a sudden change in training type or increase in training load or frequency. This sudden change does not allow the tendon to build a load tolerance to the new stimulus and tendinopathy symptoms develop. An example of this would be a lifter that has taken 2 months off from shoulder press and tries to jump back into his previous training weight with no buildup. Chronic tendinopathy often develops as a result of being exposed to repetitive loads with poor strength maintenance or inadequate rest to recover. An example of this would be a lifter that trains shoulder press 4-5 times per week incorporating poor rest between lift sessions and neglects strengthening of the smaller shoulder stabilizer muscles i.e. rotator cuff muscles.
The lifter with tendinopathy symptoms often presents with well localized shoulder pain that is initially load dependent but can progress into a constant aching pain and pain at night. There may also be a sharp pain with overhead mobility, which is referred to as shoulder impingement.
Now to understand rotator cuff injuries in relation to lifting you need a good understanding of the role of the rotator cuff. The rotator cuff consists of a series of four muscles. These muscles work together to stabilize the head of the humerus in the shoulder joint (glenohumeral joint- GHJ). The rotator cuff muscles are placed under significant stress to stabilize the GHJ during upper extremity weight lifting2.
Weight lifters often put an emphasis on targeting the larger muscle groups of the upper extremity (deltoids, pecs, trapezius), but often neglect the rotator cuff muscles. This can create an imbalance of strength between the global muscles and local stabilizing muscles in the shoulder. This miss match in combination with repetitive loading, biased exercise selection, and training errors precipitate rotator cuff tendinopathy.
Depending on the intensity, irritability and duration of symptoms a short period of time off from weight lifting may be necessary to offload the tendons. This offloading phase is closely followed by a gradual graded tendon loading program and eventual return to weight lifting. Upon return to weight training there are important modifications to consider to reduce the risk of re-injury.
We will use the bench press for example. Modifying the hand spacing and grip when returning to bench press from rotator cuff injury are instrumental in reducing the risk of re-injury. Hand spacing should be no wider than 1.5x the biacromial width (AC joint to AC joint). The narrower hand space reduced the peak shoulder torque and therefore reduces the RC and biceps tendon stabilization requirements of humeral head stabilization3,4. The narrower hand space also allows for a shoulder abduction angle less than 45 degrees and extension less than 15 degrees. This puts the pec major and biceps brachii at a mechanical advantage resulting in less stress on the RC and distal clavicle3.
In addition to hand spacing, grip type is also an important consideration in the return to lifting. The underhand grip (supination) rotates one of the RC tendons, supraspinatus, out from under the acromion, reducing the risk of impingement during the pressing motion. Whereas the overhand (pronated) grip draws the long head bicep tendon out from under the acromion but places the SSp under the acromion5.
As you can see from the literature simple consideration of hand spacing and grip type can be instrumental in the successful return to lifting of an athlete dealing with rotator cuff tendinopathy/impingement.





Anterior Shoulder Instability
An athlete may develop anterior shoulder instability as a result of previous shoulder dislocations/subluxations or a gradual insidious onset. In the athlete with previous shoulder dislocation it should be noted that a conservative management plan may not always be successful. The presence of a bony lesion to the humeral head called a Hill-sachs lesion or Bankart lesion to the gleno-humeral labrum may result in chronic instability of the shoulder joint that will result in discomfort and disability under high loads. Surgery may be indicated for this individual.
The lifter with anterior shoulder instability will present with poorly localized pain in the ‘high five’ position under load and commonly has an athletic history of overhead sports (volleyball, tennis, baseball, swimming) or previous shoulder dislocation/subluxations.
The ‘high five’ position refers to the position of the shoulder when high fiving another individual. In this position the shoulder is placed in 90 degrees of shoulder abduction and 90 degrees of shoulder external rotation. This is considered a high-risk position for individuals with anterior shoulder instability as it puts stress on the main passive primary stabilizer of the shoulder, inferior glenohumeral ligament (IGHL)6.
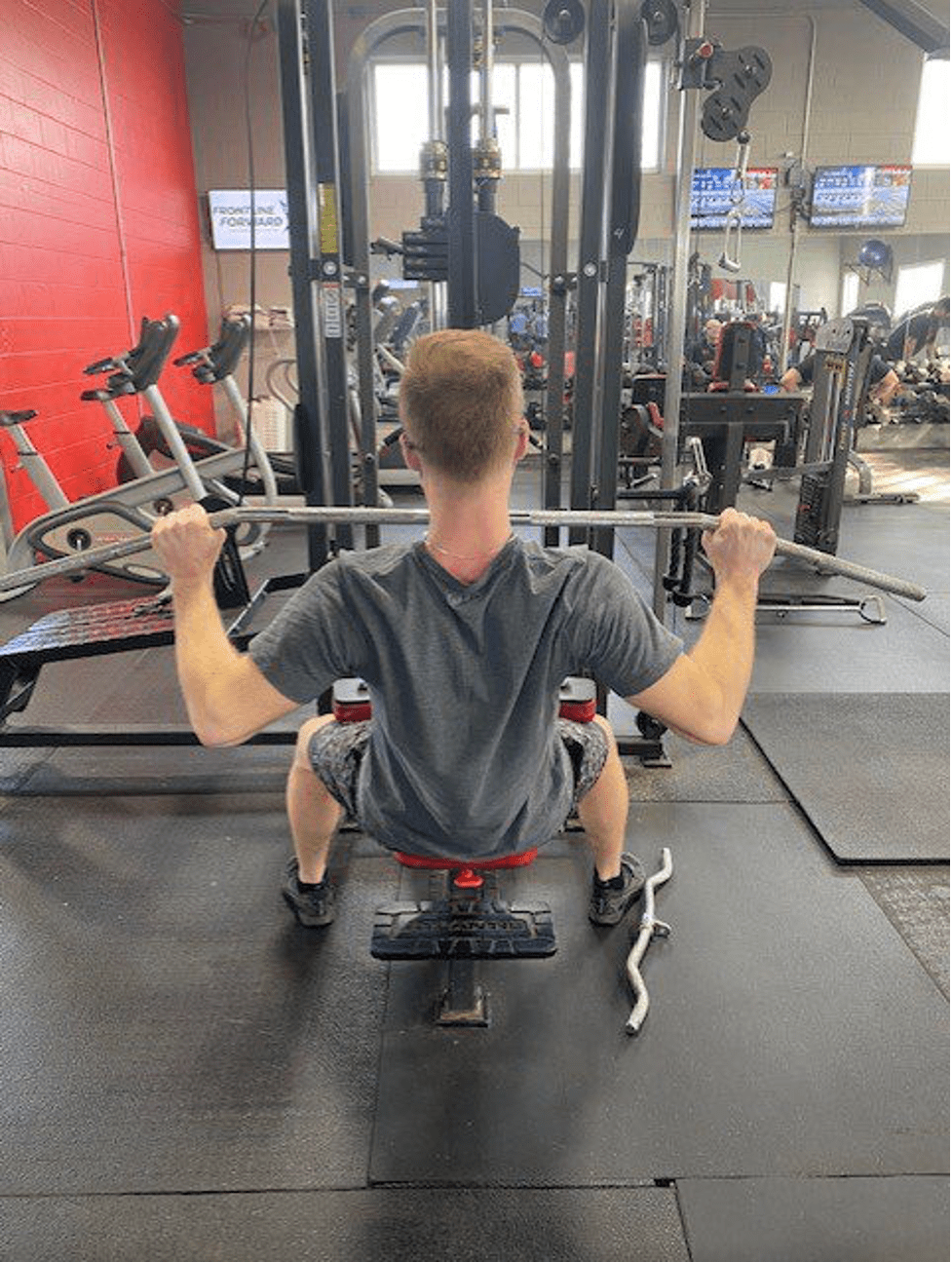
Weight lifting frequently puts the lifter in this high five position under load. This includes exercises such as the wide grip bench press, incline and supine flys, wide grip pull down, and behind the neck shoulder press. In addition, weight training is often repeated until muscular fatigue meaning that as the dynamic stabilizers of the shoulder (rotator cuff) are fatigued additional stress is placed on the IGHL and shoulder capsule6.
Treatment of the lifter with anterior shoulder instability often consists of rest from loading the high five position to settle potential inflammation in the shoulder. The lifter should be thoroughly examined to determine RC and scapular stabilizing strength prior to return to lifting.
Upon return to lifting, modifications should be put in place to avoid loading the high-risk position. We will use the behind the neck lat pull down for example. This variation of lat pull down puts an increased strain on the IGHL/anterior capsule by placing the shoulder in the high five position. A simple modification to this exercise would be to have the athlete seated with the torso declined in 30 degrees of trunk extension. This modification removes the high five position and creates better recruitment of the periscapular muscles providing increased humeral head stabilization. EMG studies also show that this position puts the lats at a mechanical advantage meaning the lifter is not sacrificing his target muscles with this modification7. Considerations of hand spacing is also important for similar reasons mentioned earlier.



Distal Clavicle Osteolysis
Distal clavicle osteolysis is often referred to as ‘weight lifters shoulder’ due to the prevalence of the condition in weight lifters. Osteolysis refers to the process of bone degeneration, where the cycle of bone uptake (osteoclast) is out competing the process of new bone formation (osteoblastic activity).
The lifter with distal clavicle osteolysis often presents with pain well localized to the distal clavicle aka AC joint


If you would like more information you can contact david@modernphysio.ca
Citations:
- Keogh JW, Winwood PW. The epidemiology of injuries across the weight-training sports. Sports Med. 2016:2016.
- Sigmon C, Tyson A: Preventing shoulder injuries by modifying the bench and incline presses. Strength Condition (August): 52-53, 1996
- Harman E: A 3D biomechanical analysis of bench press exercise [abstract]. Med Sci Sports Exerc 16: 159-160, 1984
- Wilk KE, Arrigo CE, Andrews JR: Current concepts: The stabilizing structures of the glenohumeral joint. J Orthop Sports Phys Ther 25: 364–379, 1997
- Corso G: Impingement relief test: An adjunctive procedure to traditional assessment of shoulder impingement syndrome. J Orthop Sports Phys Ther 22: 183–192, 1995
- Gross ML, Brenner SL, Esformes I, Sonzogni JJ: Shoulder instability in weight lifters. Am. J. Sports Med 21: 599-603, 1993
- Fees M, Decker T, Snyder-Mackler L, Axe MJ: Upper extremity weight-training modifications for the injured athlete: A clinical perspective. Am. J. Sports Med 26: 732-742, 1998